Research Activities
Central to the pathology in P. falciparum, the most virulent human species, is the phenomenon of cytoadherence to endothelial receptors mediated by variant surface proteins which facilitate sequestration of parasitized red blood cells deep in microvasculature. As infected reticulocytes with mature stages of P. vivax are detected in peripheral circulation, it has been amply accepted that there is no cytoadherence, hence sequestration, in deep vasculature of this human malaria parasite. Against this dogma, our group has raised evidence that P. vivax contains variant surface proteins, termed VIR, involved in cytoadherence to the spleen1 and that such cytoadherence is facilitated by interactions of extracellular vesicles from infections with human spleen fibroblasts2. Remarkably, with contributions from our group, the existence of intrasplenic infections has been recently demonstrated in prospective human studies after traumatic spleen ruptures3. In fact, it was shown that the largest parasite biomass during chronic asymptomatic infections resides in the spleen4; thus, P. vivax should now be considered a predominant infection of the reticulocyte-rich spleen and not of peripheral blood circulation. In addition to intrasplenic infections, P. vivax parasites have been suspected to reside in the BM during chronic asymptomatic infections as originally observed in the late 19th century. Morphological and molecular evidence of the parasite in this hemopoietic tissues, largely contributed by our group, have been recently observed in patients during natural infections5. Noticeably, all patients presented defects in erythropoiesis and RNAseq analysis of bone marrow aspirates from patients corroborated these morphological observations6. All together, these data call for a new paradigm in P. vivax research which will require a renewed emphasis on understanding the origin and significance of these cryptic erythrocytic niches, if elimination of malaria is to be achieved.
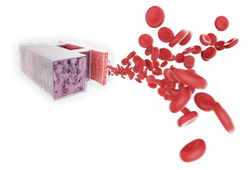
For ethical and technical reasons, working with the human spleen have been mostly limited to post-mortem analysis and studies on bone marrow aspirates are limited as it is considered a highly invasive clinical procedure. We propose implementing a disruptive technology to pursue these studies: Organs-on-a-chip (OOC) are revolutionizing personalized medicine and drug-discovery. We will construct OOC containing minimal functional units of the human bone marrow and spleen to facilitate studies of extracellular vesicles in a space and velocity that will facilitate their uptake by cells in these hemopoietic tissues and the discovery of new targets for intervention.
1. Fernandez-Becerra C, Bernabeu M, Castellanos A, Correa BR, Obadia T, et al. 2020. Proc Natl Acad Sci U S A 117: 13056-65
2. Toda H, Diaz-Varela M, Segui-Barber J, Roobsoong W, Baro B, et al. 2020. Nat Commun 11: 2761
3. Kho S, Qotrunnada L, Leonardo L, Andries B, Wardani PAI, et al. 2021. N Engl J Med 384: 2067-9
4. Kho S, Qotrunnada L, Leonardo L, Andries B, Wardani PAI, et al. 2021. PLoS Med 18: e1003632
5. Baro B, Deroost K, Raiol T, Brito M, Almeida AC, et al. 2017. PLoS Negl Trop Dis 11: e0005365
6. Brito MAM, Baro B, Raiol TC, Ayllon-Hermida A, Safe IP, et al. 2020. J Infect Dis